Cataract Awareness Month: An Interview with Dr. Hickey

This June is Cataract Awareness Month. And, in honor of the month, we sat down with Dr. Charles Hickey, our talented ophthalmologist who has been performing cataract surgery for over 30 years.
Dr. Hickey, what are some of the biggest changes in cataract surgery that have helped improve outcomes?
The two most important changes in cataract procedures have been the elimination of sutures and the ability to fine-tune refractive outcomes. Pre-operative testing of the anatomical shape and length of the eye allows us to completely eliminate distance glasses in many of our patients. We also have the option of correcting astigmatism as well as improving near vision along with good distance correction similar to what you have when wearing a pair of bifocal glasses. These are the result of improvements in the design of the small plastic lenses we place in the eye at the time of surgery.

Dr. Hickey examining patients.
What are some of the symptoms patients complain about with cataracts—besides a general blurring of vision?
Symptoms of cataracts can include difficulty distinguishing color, especially the color blue. Some cataracts act like yellow sunglasses, and people cannot distinguish navy blue from black. Having trouble with glare from bright lights is also common and can cause problems both with driving and reading. As cataracts worsen, the blur increases, making it difficult to see in all lighting conditions. It can also increase the risk of falling as patients may not see a step or curb in dim light.
While it may vary from one person to another, when is the best time to have a cataract removed?
The time to have cataract surgery is when a person is having difficulty seeing and enjoying any activity that is important to them. This varies greatly from person to person. Some cataracts blur distance vision but not reading vision. Some of these patients do not realize they have any problems at all until they flunk their vision test when renewing their driver’s license. Other cataracts cause glare and blur with reading, and these patients will often seek surgery early. It is usually an individual and personal decision made in consultation with their ophthalmologist.
Briefly, what should a patient expect on the day of surgery?
The day of surgery now starts with a COVID screening upon entering the surgical center. If all is well in this regard, patients recline on a cart, retaining their street clothes and shoes. An intravenous is started, a sedative is infused, and the area around the eye is blocked with injection medicine that the patient neither feels nor remembers receiving. They then move into the operating room on the same cart, and the surgery takes about fifteen minutes. The gentle sedative is continued, and Mozart and Beethoven play softly on WOSU radio (at least in my operating room!). The patient returns to the front area for a beverage and a snack and then leaves for home. We expect little to no pain, but some people can feel a bit of scratchiness as the eye begins to heal.
If I have had astigmatism all my life, can cataract surgery help improve that?
Patients who have lifelong astigmatism have the choice of a toric lens implant that not only corrects their distance vision but also corrects their astigmatism. This correction works much better than astigmatic glasses as the implant moves with eye movement, and patients are always using the optical center of the correction. Some of our happiest patients are those who opt to correct their astigmatism in this fashion.
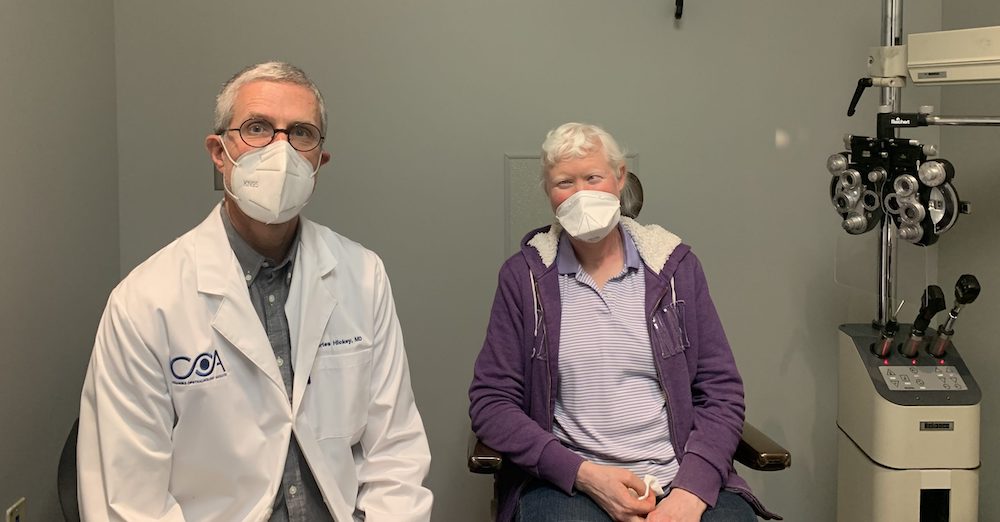
Dr. Hickey with a patient.
What are the lenses you put in the eye during surgery made of?
Lens implant materials have been greatly refined over the last thirty years and currently include synthetic materials such as acrylic and silicone. These lenses are foldable and can be inserted through very tiny surgical incisions, most under 3 mm. The lenses are permanent and should last fifty years or longer.
How successful is cataract surgery for most patients?
Cataract surgery is the most common procedure funded by Medicare, and it is the most successful. Infections and hemorrhage can be an issue, but they are quite rare. If any problem is noted during or after a procedure, prompt treatment will still result in good outcomes in most cases. It is very important however to use all pre- and post-operative eye drop medications to ensure the best results.

Dr. Hickey and a happy patient.
Can you do cataract surgery if I have macular degeneration?
Cataract surgery is commonly performed in the setting of macular degeneration. Removing the cataract will help vision but to no better than the condition that the macula allows. There are continued new improvements and medications for wet macular degeneration, and much work is being done to help dry macular degeneration as well. In time, there is hope that both types of macular degeneration can be more successfully treated.